Safety and efficacy of high dose melphalan and autologous stem cell transplantation prior to renal allograft in end-stage renal failure secondary to Monoclonal Immunoglobulin Deposition Disease
Tarun Bansal2, Rashed Hossain1, William McKane2, John A Snowden1
1Department of Haematology, Sheffield Teaching Hospitals NHS Foundation Trust, Sheffield, UK;
2Department of Renal Medicine, Sheffield Teaching Hospitals NHS Foundation Trust, Sheffield, UK
Accepted 15 March 2011
Published 16 March 2011
Summary
Monoclonal immunoglobulin deposition disease (MIDD) nearly always has renal involvement and frequently leads to end stage renal failure (ESRF). Renal transplantation is not usually considered due to an almost universal recurrence of the disease and poor survival of the renal allograft. We report the case of a 36-year-old female who was treated with induction chemotherapy followed by high dose melphalan and autologous stem cell transplantation and subsequently received a live related renal transplant from her sister. She had no rejection or major post transplant complications, and showed no signs of recurrence of disease after over 2 years of follow up. Our case suggests this mode of therapy could be considered in carefully selected patients with ESRF due to MIDD.
Keywords
Autologous stem cell transplantation (ASCT), End stage renal failure, Monoclonal Immunoglobulin Deposition Disease (MIDD), Renal allograft, Serum free light chains, Melphalan
Case Report
The treatment of Monoclonal Immunoglobulin Deposition Disease (MIDD) has not been standardized because of the small number of patients reported in the literature [3, 8, 7]. However, as MIDD is associated with plasma cell dyscrasia, patients have typically been treated with regimens used for multiple myeloma, most commonly melphalan and prednisolone. In the largest series of patients, seven patients with MIDD were treated with high dose melphalan and autologous stem Cell Transplant (ASCT), some prior to renal allograft, with beneficial results3.
To add to this preliminary experience, we report on a 36-year-old female, originally referred to the renal unit in April 2006 with hypertension and nephrotic range proteinuria (24 hr urine protein 4.69g, serum albumin 40g/l) and an elevated serum creatinine (380umol/L). She had several small palpable lymph nodes but no splenomegaly. Urine protein immune electrophoresis showed kappa monoclonal free light chain 0.04g/l. A renal ultrasound scan was normal and a CT thorax, abdomen, and pelvis showed no evidence of lymphoma. A renal biopsy confirmed nodular glomerulosclerosis and monotypic staining for kappa on immunofluorescence. Electron microscopy showed nodular glomerulosclerosis, numerous medium to large heterogeneous electron dense deposits in paramesangial areas, linear densities on the endothelial side of the glomerular basement membrane with similar electron dense material seen at the periphery of the arterioles, and membranes suggestive of MIDD at the periphery of the tubular basement. In association, criteria for myeloma were fulfilled based on Kappa Bence Jones proteinuria (0.04g/l), kappa serum free light chains (1000 mg/l) and 13% atypical plasma cells on bone marrow examination. Immunoglobulin immunofixation showed no serum monoclonal immunoglobulin, but immune paresis was confirmed. A SAP scan showed no evidence of light chain deposition or amyloidosis in other organs. The patient progressed to end stage renal disease and was initiated on peritoneal dialysis and subsequently transferred to hemodialysis via an arteriovenous fistula in February 2007. The plasma cell dyscrasia was treated with attenuated cyclophosphamide, thalidomide, and dexamethasone (CTD regimen) without significant complications and a good partial response was achieved after six cycles (January – June 2008).
Given her age and otherwise good performance status, the long-term strategy of a renal allograft was considered reasonable. It was logical to consider that maximal suppression of the plasma cell dyscrasia for the longest period would offer the best protection of a potential renal allograft from MIDD. High-dose melphalan and autologous stem cell transplant (ASCT) is a standard of care in myeloma patients which offers a prolonged treatment-free period and high chance of a complete remission that is associated with immunofixation negativity. Although feasible in patients with renal failure, the treatment-related mortality is significantly higher [7]. Clinical review confirmed her fitness to proceed with high-dose melphalan and ASCT, and after weighing up the risks and benefits, the patient consented to the procedure.
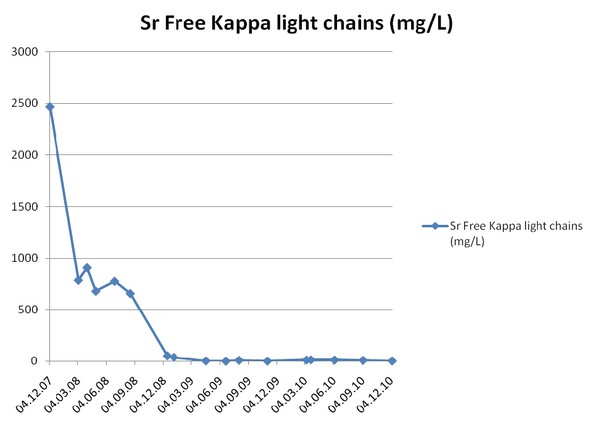
Peripheral blood stem cells were successfully harvested with G-CSF 10mcg/kg subcutaneously and apheresis. In September 2008, the patient was admitted for high dose melphalan and ASCT. Hemodialysis was performed on the day prior to inpatient admission (day –3), admitted and received high dose melphalan 140mg/m2 (day –2), hemodialysed on day –1, and underwent autologous stem cell infusion (2.86x10*6/kg CD34+ cells) and hemodialysis on day 0. No major complications occurred following stem cell infusion apart from the routine toxicities (vomiting, diarrhea, vaginal thrush, cytopenia, and upper GI mucositis). Neutropenic sepsis was successfully treated with broad-spectrum antibiotics (meropenem and vancomycin). The response to HDM and ASCT was assessed at around day +100 (Jan 6, 2009) following the procedure. A bone marrow aspirate and trephine biopsy examination on day 100 post stem cell infusion showed no excess of plasma cells (1%). Serological responses to induction treatment and autologous transplant are summarized in Fig. 1, confirming an excellent prolonged response after SCT.
Figure 1. Serum Free kappa light chain assay
In March 2009, the patient underwent a live related renal transplant from her sister (112 mismatch, CMV negative-negative). A low level HLA donor specific antibody (DSA) was detected in the recipient serum by Luminex single antigen beads (DR 17) both before and after the high dose melphalan. Flow cytometric crossmatching with T and B cells was negative. Thymoglobulin induction was considered too hazardous in the context of recent high dose melphalan and immune paresis. A standard immunosuppression regime of prednisolone, tacrolimus, and mycophenolate mofetil (MMF) with Basiliximab induction was used. There were no immediate complications and she was discharged one week later. Tacrolimus doses were adjusted according to whole blood levels; target level 8–12ug/l. A renal allograft biopsy in April 2009 showed no evidence of rejection or recurrent disease, but electron microscopy was not performed. She had a period of chronic diarrhea but no evidence of CMV colitis on sigmiodoscopy and rectal biopsy. MMF was switched to mycophenolate sodium and the diarrhea resolved. She developed BK viruria (peak level >1,000,000 viral copies/ml) and low level viremia (50 viral copies/ml) associated with graft dysfunction nearly one year after her renal transplant. A biopsy was not performed but her immunosuppression was reduced to aim for a tacrolimus level between 3–4 µg/l. There has been no recurrence of proteinuria; recent serum creatinine was 110 umol/l. The only late effect of the chemotherapy and transplant procedures has been a premature menopause requiring hormone replacement therapy (osteoporosis on bone mineral density scan), although this required cessation due to fluid retention and was replaced with weekly alendronic acid. ECG and echocardiography have shown no long-term cardiac dysfunction (cardiac investigations were done to monitor cardiotoxicity from treatment). As of December 2010, the patient continues under regular joint follow up with hematologists and nephrologists, and has successfully returned to work with normal performance status.
Discussion
Renal involvement is considered universal in patients with MIDD [7, 9, 10]. It classically present as nodular mesangial sclerosis, thickening of glomerular basement membrane, and mesangial expansion, with endocapillary proliferation being other common findings, though diagnosis is usually confirmed with electron microscopy, which can demonstrate granular electron-dense deposits located with in the tubular basement membrane, glomerular basement membrane, vessel wall and also mesangium [10]. Renal transplant is generally not considered in these patients due to an almost universal recurrence of the disease and poor survival of renal allograft [4]. For patients with MIDD who do not have multiple myeloma, the median allograft survival rate is only 37.5 months. This increases to 47.9 months if deaths with a functioning graft are excluded, but it is far from the 12.5 to 19.9 years projected for median allograft survival rate in patients without MIDD [6]. Renal allograft survival could be prolonged by achieving good hematological remission. Recently this has been achieved by using high dose chemotherapy followed by ASCT, though no evidence is available in control settings [5, 1, 2]. It is therefore logical to aim for maximal suppression of light chain production and delay in recurrence of disease in renal allograft. An additional interest of this case is the fact that the high dose melphalan did not abrogate the allosensitization. However, despite the presence of a DSA and standard immunosuppression the recipient did not experience rejection.
This case adds to the limited literature regarding the management of MIDD with intensive anti-myeloma treatment, including the feasibility of consolidation with high dose melphalan and ASCT as a means of achieving as deep a remission as possible prior to renal allograft. The goal of successful therapy may hinge on the complete suppression of light chain production and, in view of this; an excellent clonal response has been sustained for over two years following the high dose melphalan and ASCT. Clearly, long- term follow up of all such cases is necessary to evaluate the efficacy of high dose melphalan and ASCT and other anti-myeloma treatments in the protection of the renal allograft from the re-emergent MIDD, and also in relation to how close monitoring may extend this protection by guiding the early re-introduction of second line therapies, including novel agents such as bortezomib and lenalidomide, or even further SCT procedures. Given the rarity of MIDD, further reports of such cases would be valuable. Multi-centre registry based studies may help address these questions.
Acknowledgements
The authors have declared that no competing interests exist.
References
2. Bird JM, Owen R, D’Sa S, Snowden J, Pratt G, Ashcroft J, Yong K, Cook G, Feyler S, Davies F, Morgan G, Cavenagh J, Low E, Behrens J. Guidelines for the diagnosis and management of multiple myeloma 2010. British Journal of Haematology, in press.
3. Dhodapkar MV, Merlini G, Solomon A. Biology and therapy of immunoglobulin deposition diseases. Hematol Oncol Clin North Am. 1997;11:89-110.
5. Firkin F, Hill PA, Dwyer K, Gock H. Reversal of dialysis dependent renal failure in light-chain deposition disease by autologous peripheral blood stem cell transplantation. Am J Kidney Dis. 2004;44:551-555.
8. Heilman RL, Velosa JA, Holley KE, Offord KP, Kyle RA. Long-term follow-up and response to chemotherapy in patients with light-chain deposition disease. Am J Kidney Dis. 1992;20:34-41.
10. Leung N, Lager DJ, Gertz MA, Wilson K, Kanakiriya S, Fervenza FC. Long-Term Outcome of RenalTransplantation in Light-Chain Deposition Disease. Am J Kidney Dis. 2004;43:147-153.
Accepted 15 March 2011
Published 16 March 2011


